Heartburn Overview
Heartburn is a common condition that affects millions of people every year. It is characterized by a burning sensation in the chest, typically after eating, or when you lie down at night. It can be caused by various factors, including diet, lifestyle, underlying health conditions, high stomach acid, and even low stomach acid. Understanding the causes of heartburn and making lifestyle modifications can help manage symptoms and improve overall digestive health.
Symptoms of Heartburn:
The most common symptom of heartburn is a burning sensation in the chest, typically after eating. Other symptoms may include a sour or bitter taste in the mouth, a persistent cough, changes in singing voice, and difficulty swallowing. Some people can have acid reflux with no symptoms at all.
It’s important to pay attention to the timing of your heartburn and what it means. If heartburn occurs while you eat, then it’s likely caused by high stomach acid. However, if heartburn comes on after you eat, especially hours after, and with other symptoms, it’s likely caused by low acid, poor digestion, and/or issues with gut movement. Along those lines, one of the most common conditions to occur alongside heartburn is indigestion, also called dyspepsia. Indigestion can cause heartburn/burning feelings in the stomach, feeling of fullness hours after eating, nausea, and pain.
Causes of Heartburn:
Heartburn can be caused or worsened by various factors, including dietary triggers, lifestyle factors, and underlying health conditions. Heartburn is a common symptom in indigestion, impaired stomach function, and gut structural issues. Some common triggers of heartburn include:
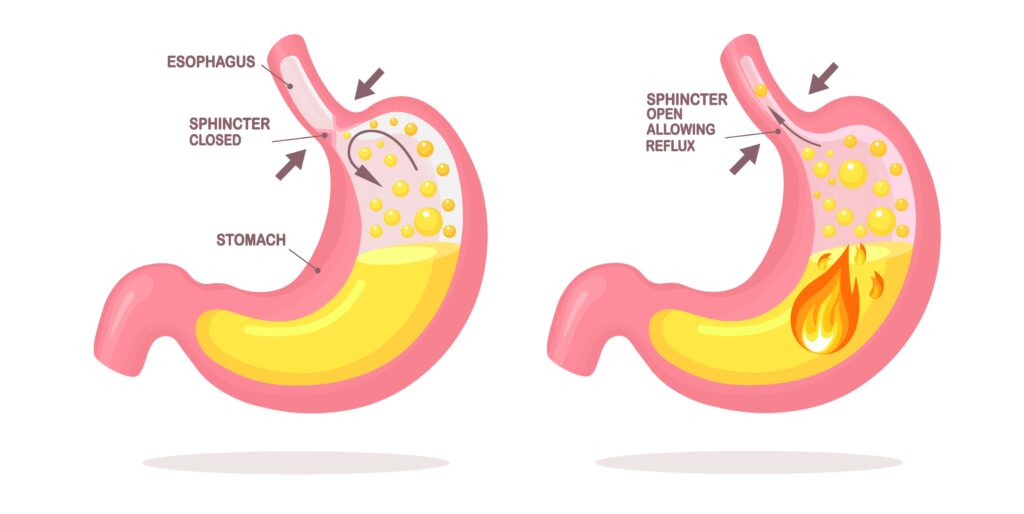
- Poor digestion due to low acid and/or low digestive enzymes: Contrary to popular belief, low stomach acid levels commonly contribute to heartburn. When stomach acid is insufficient, it can lead to incomplete digestion of food, inability to kill organisms swallowed with food, delayed stomach emptying, and increased gas pressure from fermentation, all of which can contribute to heartburn. Even though there’s low acid, the pressure can still force acid up into your throat, causing the symptoms of heartburn.
- Too much “bad” bacteria: overgrowth of “bad bacteria”, such as H. pylori, and decrease in “good” bacteria can trigger low acidity, poor digestion, and heartburn. In addition, your “good” bacteria produce serotonin so your gut can move properly, and recent research indicates poor gut bacteria is heavily linked to stomach pain, hypersensitivity to pain, and feeling uncomfortably full long after a meal.
- Stress: Excess stress can block your digestive system from working properly, including being able to digest your food, relax the muscles necessary for digestion, and moving food out of your stomach at a healthy pace.
- Consuming alcohol, caffeine, mint, chocolate, citrus, spicy or fatty foods: these foods can relax the valve that holds food down or cause additional pressure, allowing stomach acid to flow back into the esophagus and cause heartburn.
- Eating large meals or lying down right after eating: Eating large meals can put pressure on the stomach and push stomach acid back into the esophagus. Lying down right after eating can also increase the risk of heartburn.
- Being overweight or obese: Excess weight can put pressure on the stomach and lead to heartburn.
- Smoking: Smoking can weaken the lower esophageal sphincter, allowing stomach acid to reflux into the esophagus and cause heartburn.
- Pregnancy: Hormonal changes during pregnancy can relax the lower esophageal sphincter, increasing the risk of heartburn.
- Hiatal hernia: A hiatal hernia is a condition where a part of the stomach protrudes into the chest cavity through the diaphragm, which can contribute to heartburn.
What Can You Do?

Addressing heartburn is multifaceted. It’s important to consider why you may be having heartburn and what could be making it worse. While there is no one-size-fits-all approach to treating heartburn, dietary modifications can help manage symptoms. Some dietary and lifestyle recommendations for heartburn management include:
- Supporting your digestive system by reducing stress, consuming pre and probiotic foods such as fermentable fibers and fermented foods, and taking digestive enzymes.
- Avoiding triggers, such as spicy or fatty foods: Identifying and avoiding foods that trigger heartburn can help reduce symptoms.
- Eating smaller, more frequent meals: Eating smaller meals throughout the day instead of large meals can help prevent stomach pressure and reduce the risk of heartburn.
- Avoiding lying down right after eating: Waiting at least 2-3 hours after eating before lying down can help prevent stomach acid from refluxing.
- Maintaining a healthy weight: Maintaining a healthy weight can help reduce pressure on the stomach and lower the risk of heartburn.
- Drinking plenty of water: Staying hydrated is important for proper digestion and stomach function, but limit fluid intake during meals to ½ glass so you don’t dilute your stomach acid.
Supplements to Support Heartburn and Discomfort
In addition to dietary changes, there are several supplements that can help manage heartburn symptoms. We have a full protocol we use in our practice, and some recommendations include:
Digestive enzymes:
Digestive enzymes can help break down food and improve digestion, reducing the risk of heartburn. This can be especially helpful if your heartburn comes on hours after a meal. We like this product because it combines bile, stomach acid, and enzymes for robust digestive support.
Deglycyrrhizinated licorice (DGL):
DGL can soothe the digestive tract and reduce inflammation, providing relief from heartburn. DGL can be used regardless of cause of heartburn and works best when used as a lozenge.
Probiotics:
Probiotics can improve gut health and balance gut bacteria, which can help prevent heartburn and promote overall digestive health.
(You can view the whole protocol with full instructions here)
Common drugs used for heartburn can provide short-term relief by reducing stomach acid production or neutralizing acid. However, it’s important to note that these medications are not intended for long-term use due to potential risks and side effects. Prolonged use can lead to reduced nutrient absorption and increased risk of bone fractures, kidney disease, and other health issues. Approaches such as diet, lifestyle, and supplementation may be appropriate for long-term management of heartburn symptoms with reduced risks.
Heartburn may be common, but that doesn’t mean you have to live with it. If you feel you need additional support or just have questions, please don’t hesitate to reach out and ask to speak with our pharmacist or a clinical nutritionist.
References:
Graham DY, Ketwaroo GA, Money ME, Opekun AR. Enzyme therapy for functional bowel disease-like post-prandial distress. J Dig Dis. 2018 Nov;19(11):650-656. doi: 10.1111/1751-2980.12655. Epub 2018 Sep 21. PMID: 30101562; PMCID: PMC6910206.
Cheng J, Ouwehand AC. Gastroesophageal Reflux Disease and Probiotics: A Systematic Review. Nutrients. 2020; 12(1):132. https://doi.org/10.3390/nu12010132
Tziatzios G, Gkolfakis P, Papanikolaou IS, Mathur R, Pimentel M, Giamarellos-Bourboulis EJ, Triantafyllou K. Gut Microbiota Dysbiosis in Functional Dyspepsia. Microorganisms. 2020 May 8;8(5):691. doi: 10.3390/microorganisms8050691. PMID: 32397332; PMCID: PMC7285034.
Swami OC, Shah NJ (2017) Functional dyspepsia and the role of digestive enzymes supplement in its therapy. Int J Basic Clin Pharmacol 6(5):1035–1041